By: Dr. Anuja Mathew, DPT, MsPT, OCS – Orthopedic and Pelvic Floor Physical Therapist
First, I would love to introduce myself if you don’t already know me. My name is Dr. Anuja Mathew and I am a licensed Physical Therapist in the states of New York and New Jersey. I am board-certified in Orthopaedics, with an Orthopedic Clinical Specialist certification (one that is earned by 5% of Physical Therapists across the country – not to toot my own horn), as well as trained in Women’s Health/Pelvic Floor. I’ve been in practice for over 10 years now, and am a strong promoter of manual therapy, therapeutic exercises, and biofeedback. I have been treating patients with orthopedic conditions such as sports injuries, tendonitis, arthritis, lumbar/cervical pain, and post-surgical rehabilitation. I also have experience in Women’s Health conditions such as Urinary Incontinence, pelvic pain, pubic symphysis dysfunction, diastasis recti, and prenatal and postnatal rehabilitation.
Congrats on being pregnant! Many people struggle to get to where you are, so be proud! Motherhood is a fun and rewarding journey, but it can also be a tough one. Many soon-to-be and new mothers might experience pain in places they haven’t experienced before, and working through those pains can be a challenging journey. This rewarding chapter in your life may also come with some unwanted side effects like lower back pain, soreness, or pelvic pain. These often occur during prenatal carrying and postpartum delivery. Physical therapy can help with any pains that might’ve popped up during this time, but it can also help you have a smoother pregnancy and birth in general.
A woman’s body is constantly changing during pregnancy. This increase in weight may cause an increased strain on the spine, along with the increased ligament laxity could cause pain and instability in the lumbar and thoracic spine and pelvis. The pelvic floor is a complexity of joints, ligaments, connective tissue, and muscles. All of which can be affected due to numerous reasons which cause tightness, weakness, and pain in your body.
Some common questions we get are during one’s pre or postnatal journey include:
1) Is it normal to have back low back pain during pregnancy? How can I prevent sciatica?
Some discomfort in your lower back is normal during pregnancy. In fact, the American Pregnancy Association reports that 50-70% of women experience back pain while pregnant. As your ligaments stretch and your pelvis widens, you will feel some discomfort in the first trimester. As your belly grows, the center of gravity shifts and this causes increased strain on your lower back. Anything more than just discomfort should be addressed right away. Sciatica is one of the more common diagnoses during pregnancy. A lot of times it could be pelvic girdle pain that is misinterpreted as sciatica. It would help to do some strengthening of your hip muscles to improve stabilization in your pelvis and reduce the pelvic girdle pain.
2) What exercises can be done during pregnancy to reduce low back pain? Do’s and Don’ts.
Exercises done during pregnancy should focus on hip strengthening, and gentle stretches for the lumbar spine, hamstrings, adductors, and glutes. Prenatal yoga is usually safe to perform.
Do not perform any abdominal exercises like crunches or sit-ups, as it might make your diastasis worse, and to be honest — there is a very little chance that you will get 6-pack abs while your belly is growing. If you have been a runner prior to pregnancy, you can continue running, but be careful in your 1st and 3rd trimester. A belly belt/support should be worn or Kinesio-taping should be done to prevent diastasis during your prenatal and postpartum journey.
Other good measures to take are strengthening your upper body during breastfeeding, as you most likely will have poor posture that might lead to upper back and shoulder pain. Maintaining good posture during pregnancy with postural awareness, strengthening, and stretching is a MUST. Though the Kegel is a good exercise to start during pregnancy, it is not always advisable for all pregnant patients. People suffering from vulvodynia, dyspareunia, or pelvic pain should focus on reverse Kegels and relaxation more than performing regular Kegel exercises.
3) Am I at risk for gestational diabetes?
Doing regular, gentle exercises, and walking can prevent gestational diabetes. So just remember to stay active during your pregnancy, and you should be good to go!
4) How do I stop urine from leaking when I don’t want it to. And when should I go to the doctor/physical therapist?
Performing pelvic floor strengthening is not just in the form of Kegels but other strengthening methods integrated with core strengthening can prevent leakage.
If you notice any pressure in your vagina, any bulging from your vagina while passing urine or otherwise, you will need to consult your physical therapist or OBGYN to rule out pelvic organ prolapse. If the leakage of urine has prolonged for more than 6 weeks postpartum and is getting worse, then you need to see your physical therapist.
5) You guys can improve scar tissue? What benefits does that have besides aesthetic reasons?
Physical therapy can help with scar tissue mobility for C-section scar, episiotomy scar, or scarring from a 1st-3rd degree tear. Scar tissue causes fascial restriction, which means it can adhere to the surrounding soft tissue and organs. This will often cause pain, poor extensibility, and decreased strength in the area.
You should wait until 6 weeks postpartum to start massaging or mobilizing your scar tissue.
6) How can I get rid of this split down my ab muscles?
That split or gap is known as Diastasis Recti, which is the separation of the abdominal muscle. During pregnancy, the uterus moves up into the abdomen and stretches between the rectus abdominis muscles to make room for the growing baby. Diastasis Recti can cause low back or pelvic pain but don’t worry, a physical therapist can help in reducing this separation through soft tissue mobilization in the abdomen, strengthening techniques, and even breathing techniques!
Some things to remember during pregnancy to avoid diastasis are: do not perform abdominal crunches and use Kinesio tape or a belly support belt during your 2nd and 3rd trimesters.
Here’s how to perform a self-test at home to see if you have Diastasis: Lay on your back, lift head off the ground, leaving your shoulders resting. Take your fingers and feel down the central abdomen, beginning at the sternum and travel all the way down while assessing that central line until you hit your pubic bone. While feeling down the midline, here’s what to look for:
- How wide is your separation?
- How deep is it?
- Can you feel the walls on either side of the separation?
- Is there any bulging in your central abdomen as you lift your head? (if you do see bulging, it is a sign that there is significant weakness in the deep layers of the abdomen)
7) Sex hurts. Will it always be like this? When does the pain go away?
This is known as Dyspareunia, which is a recurrent pain that is often located in the genital area and may occur before, during, or after sexual activity. This pain might come on as a result of the way your body changes during pregnancy, infections/STIs, vaginal dryness, or just stress. But luckily there are things you can do at home, or we can do to help Dyspareunia. Simple stretches like child’s pose, happy baby, along with diaphragmatic breathing and pelvic floor relaxation can go a long way. Pelvic floor massages and the trigger point release method using your finger, pelvic wand, or a miracle ball can help your symptoms as well. Pelvic wands and miracle balls are available online for purchase, however, we would not advise using these during pregnancy.
8) What is Pubic Symphysis Dysfunction and how do I know if I have it or am at risk for it? What can help these symptoms?
Pubic Symphysis Dysfunction is when your ligaments that normally keep your pelvic bone aligned during one’s pregnancy become too relaxed and stretchy after childbirth. This causes the pelvic joint – or symphysis pubis – to be unstable and which in turn, causes pelvic pain. Some symptoms include difficulty while walking and pain in your pelvis, typically focused in the pubic area but can also radiate towards the upper thighs and perineum. This doesn’t only happen while walking, but can happen while one is lifting heavy items, climbing stairs, getting dressed, getting into your car, or even while in bed.
You can do many things to ease your discomfort. We would recommend Hip stabilization exercises during pregnancy and also using an SI loc belt. Avoiding triggers is also important, this includes keeping your knees together during transfers like getting out of a car or getting out of bed, sitting down while getting dressed, and avoiding heavy lifting.
9) Why do I need a Pelvic PT for my pre-natal/post-natal care when I already have an OB/GYN that I go to?
An OBGYN is usually the first doctor people think of when it comes to prenatal care, delivery, and the postpartum journey. However, they usually aren’t trained to address the musculoskeletal implications like a Physical Therapist is. A Pelvic Floor Physical Therapist is even more apt to treat your pains and discomforts if you are pregnant, just gave birth, or just have any pelvic pains that might be also causing your abdomen, back or hip pain. However, not all OBGYNs will know when to refer their patient to a Pelvic Floor Physical Therapist, which is why often we encourage people to ask for a referral from their physician themselves. Some OBGYNs still may not give a referral, but you can always come straight to us and we can give you a free consultation!
No one deserves to live in pain, and the best way to help it is to prevent any further complications from happening. We believe in Preventative health as much as Reactive health, which is why seeing a Pelvic Floor Physical Therapist is important, especially while pregnant, to prevent any pain or conditions from happening in the first place. Here’s to healthy pelvic floors, and tearing down the stigmas that often surround Women’s Health issues!
Do you pee when you laugh? Or often feel like you won’t make it to the toilet on time?
That might be Urinary Incontinence. Urinary Incontinence is any undesired leakage of urine and the loss of bladder control, which is a common problem that affects both men and women. According to the American Urological Association, one-quarter to one-third of men and women in the United States experience Urinary Incontinence.
There are different types of Urinary Incontinence which includes:
- Stress Incontinence – urinating when putting pressure on bladder by coughing, sneezing, exercising, laughing, or lifting heavy.
- Urge Incontinence – having an intense urge to urinate, followed by involuntary loss of urine. Includes urinating throughout the night.
- Overflow Incontinence – having frequent dribbling of urine because of a bladder that doesn’t empty completely.
- Functional Incontinence – physical or mental impairment that prevents you to be able to get to the toilet on time. An example is arthritis that gets in the way of
- Mixed Incontinence – experiencing more than one type of incontinence, as listed above.
There is a long list of factors that can cause it, which includes childbirth, abdominal weakness, diabetes, pregnancy, menopause, and more. It can also be an uncomfortable topic for some, despite it being a widespread condition! Those who are pregnant may also experience persistent Urinary Incontinence due to hormonal changes, and the growing weight of the fetus which can lead to stress incontinence.
But you don’t have to live in pain. Did you know physical therapy can actually help? Specifically, seeing a Pelvic Floor Physical Therapist. A Pelvic Floor PT can help you create an individualized treatment program to help you improve your pelvic-floor muscle function. One can also help you improve control over your symptoms, as well as reduce the need for pads or incontinence medications, or even surgery! It’s much more than muscle strengthening when it comes to overcoming your Urinary Incontinence, it could also be about coordination, muscle imbalances, incorrect posture, core weakness, or even tight, overly active muscles.
Give us a call today if you or someone you know is experiencing or has been diagnosed with Urinary Incontinence and let’s figure it out together.
And how can it help you?
An Orthopedic Physical Therapist specializes in treating conditions that affect your musculoskeletal system. It involves many hands-on techniques, manual therapy, and exercises to improve many things – such as flexibility and strength of muscles, increasing range of motion of joins, reducing inflammation in joints and tendons, as well as reducing scar tissue post-surgery. This means that Orthopedic PTs can treat almost any condition that affects your ability to move or physically function in your everyday life.
What does your musculoskeletal system include? It includes your ligaments, tendons, joints, muscles, bones, and all connective tissue.
So what are some conditions that affect the musculoskeletal system?
- Arthritis
- joint pain
- knee instability
- limited range of motion
- lower back pain
- frozen shoulder
- scoliosis
- stroke
- plantar fasciitis
- muscular dystrophy
Orthopedic Physical Therapists also help a lot of patients who are recovering after surgeries. This is to help reduce pain, improve walking or a limited range of motion, and scar tissue.
Patients often need an Orthopedic PT after surgeries/injuries like:
- rotator cuff repair
- knee replacement
- hip replacement
- herniated disk
- sprained ankle
- torn meniscus
- shin splints
- tennis elbow
- carpal tunnel
So don’t wait to get checked up by an Orthopedic certified Physical Therapist. One can analyze your movement to find the source of injury or problem. They can improve pain, swelling, stiffness, immobility, as well as give you advice on preventing injuries in the future.
If you suffer from any of the aforementioned problems, give us a call today to get treated by Dr. Mathew.
Fun Fact: Did you know she has been awarded the Orthopedic Clinical Specialist (OCS) certification by the American Board of Physical Therapy Specialists? A specialization that requires thousands of hours of training and is earned by only 5% of Physical Therapists across the country.
If you or someone you know has ever suffered from pain during sex, sitting for a long amount of time, or wearing tight pants, you might be scratching your head as to the root of your pain. You may think it’s a urinary tract infection, or maybe even an STD. But when the tests are negative, you and your healthcare provider may not be aware that this pain could be thanks to musculoskeletal dysfunction, which can be treated by a pelvic physical therapist.
Your pelvic floor is a set of muscles that support the bladder, bowel, rectum, and uterus. Pelvic floor pain is something that is not talked about enough in our everyday lives and on social media. Women can suffer from pelvic floor pain, and not even know it! In many cases, bladder, bowel, or pelvis symptoms may be occurring due to problems with the muscles, joints, nerves, or connective tissues in that area.
Pelvic floor physical therapy can help with many different kinds of problems including:
- Frequent urination
- Urgency: Strong urge to urinate
- Incontinence: Unwanted leaking of urine or stool
- Constipation
- Overactive or weak pelvic floor muscles
- Endometriosis
- Menopause
- Pain in the pelvis, hip, abdomen, low back
- Painful intercourse
- Sexual dysfunction
- Pregnancy/post-pregnancy pain or intercourse
- C-section recovery
- Pelvic Organ Prolapse
- Vulvodynia
- Bladder pain syndrome
- Tailbone Pain
- Postsurgical rehabilitation
These symptoms may be caused by the strength of the pelvic floor and associated muscles and structures. Thus, the movement, muscle tone, and strength of your low back, hips, abdomen will be assessed, together with your posture and alignment. Pelvic floor physical therapists can treat many different conditions and can help you keep your pain in check. Women need to know that pelvic pain isn’t normal during menopause or any other time. Also, the longer one experiences chronic pain, the more likely nerve receptors will become sensitized to it.
Here at New York Plaza Physical Therapy, we wish to open that dialogue about the countless people, especially women, who suffer from pelvic pain and provide some treatment options to assist them in living a pain-free life. We understand that the implications of pelvic pain going unnoticed or unchecked can deeply affect one’s quality of life. So if you’re stricken by unexplained chronic pelvic pain or any of the above symptoms, it may be wise to give us a call today.
References:
Harvard Health Publishing. (2020, October 13). Pelvic physical therapy: Another potential treatment option. Retrieved from https://www.health.harvard.edu/womens-health/pelvic-physical-therapy-another-potential-treatment-option
Tate, L. (n.d.). What in the World is Pelvic Floor Physical Therapy? Retrieved December 18, 2020, from https://www.pennpartners.org/blog/expertise-general-outpatient-therapy-pelvic-floor-physical-therapy-specialty/what-world-pelvic
WHETHER YOU’RE BACK IN THE OFFICE OR WFH, THESE CAN EASILY BE DONE FROM ANYWHERE 👩💻
Work-related injuries aren’t limited to people who work with heavy manufacturing or construction. They can occur in every industry and work environments, including office spaces. Studies have proven that repetitive motion, poor posture, and staying in the same position for long periods of time can cause or worsen musculoskeletal disorders. Make sure to take a break every hour or so to stretch out and move your body.
Below are some easy exercises anyone can do at the workplace!
Cervical Retraction
These movements are meant to correct forward head posture. You are retraining deep cervical flexors while maintaining mobility in the cervical spine. This will prevent disc herniation and degeneration.
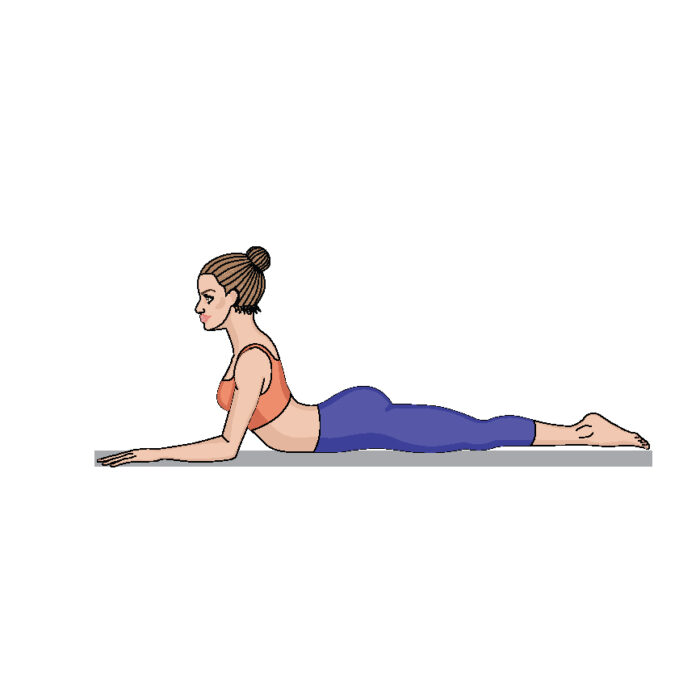
Lumbar Extension
This exercise prevents lower back pain. Sitting causes increased rounding of the lumbar spine and increased risk of disc herniations. The extension helps maintain mobility in the spine.
Scapular Retraction
Here we use shoulder blade pinching to correct slouching posture. Bring your shoulder blades together, hold for 5 seconds, and relax.
Wrist Flexors
Do you want to prevent Carpal Tunnel Syndrome and Tendinosis of the wrist? All you need to do is hold each stretch for 20 seconds.
5 Simple Ways To Prevent Back Pain
A study shows that 3/5people suffer from either neck pain or back pain or both.
A recent study from American Journal of Public Health, reveals that 1 hour of siting = 1 cigarette..
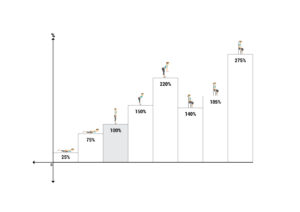
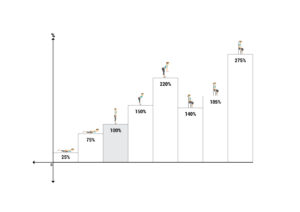
Here is a chart that will give you an insight on how much pressure falls on the disc during various activities that we carry on during the day. Unsupported sitting put maximum pressure on the spine which results in pain.
Symptoms of back pain depending on the severity of your condition:
- Centre back pain
- Pain radiating to either or both legs
- Tingling or numbness in either or both legs
- Weakness of leg muscles
How can you prevent pain & treat yourself:
- Maintaining a correct posture
- Using a Lumbar roll while sitting
- Taking adequate breaks – every 30mins for 30seconds
- Bend from the knees not back
- Strengthening your spinal muscles
We bend about 7000+ times a day which loads the spine more leading to back pain.
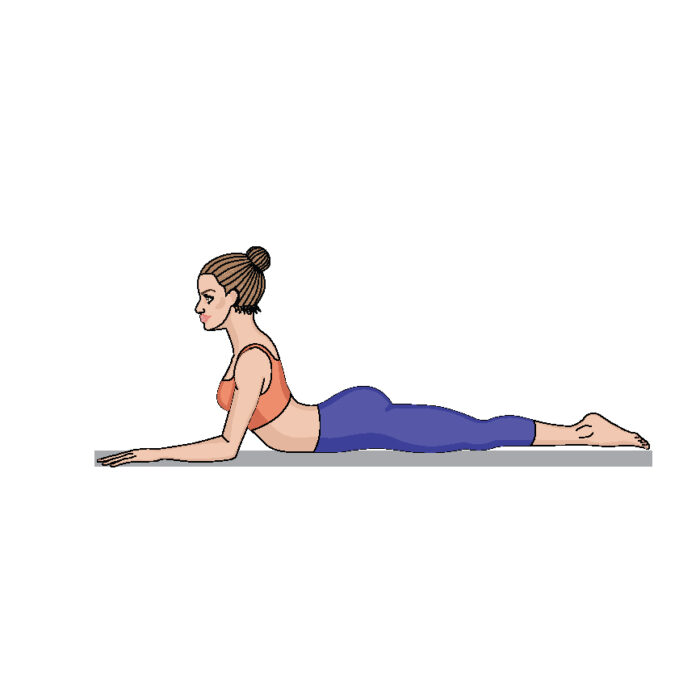
This simple exercise can help you alleviate the pain and relieve the extra stresses that fall on the spine.
By: Dr. Anuja Mathew, DPT, MsPT, OCS – Orthopedic and Pelvic Floor Physical Therapist
First, I would love to introduce myself if you don’t already know me. My name is Dr. Anuja Mathew and I am a licensed Physical Therapist in the states of New York and New Jersey. I am board-certified in Orthopaedics, with an Orthopedic Clinical Specialist certification (one that is earned by 5% of Physical Therapists across the country – not to toot my own horn), as well as trained in Women’s Health/Pelvic Floor. I’ve been in practice for over 10 years now, and am a strong promoter of manual therapy, therapeutic exercises, and biofeedback. I have been treating patients with orthopedic conditions such as sports injuries, tendonitis, arthritis, lumbar/cervical pain, and post-surgical rehabilitation. I also have experience in Women’s Health conditions such as Urinary Incontinence, pelvic pain, pubic symphysis dysfunction, diastasis recti, and prenatal and postnatal rehabilitation.
Congrats on being pregnant! Many people struggle to get to where you are, so be proud! Motherhood is a fun and rewarding journey, but it can also be a tough one. Many soon-to-be and new mothers might experience pain in places they haven’t experienced before, and working through those pains can be a challenging journey. This rewarding chapter in your life may also come with some unwanted side effects like lower back pain, soreness, or pelvic pain. These often occur during prenatal carrying and postpartum delivery. Physical therapy can help with any pains that might’ve popped up during this time, but it can also help you have a smoother pregnancy and birth in general.
A woman’s body is constantly changing during pregnancy. This increase in weight may cause an increased strain on the spine, along with the increased ligament laxity could cause pain and instability in the lumbar and thoracic spine and pelvis. The pelvic floor is a complexity of joints, ligaments, connective tissue, and muscles. All of which can be affected due to numerous reasons which cause tightness, weakness, and pain in your body.
Some common questions we get are during one’s pre or postnatal journey include:
1) Is it normal to have back low back pain during pregnancy? How can I prevent sciatica?
Some discomfort in your lower back is normal during pregnancy. In fact, the American Pregnancy Association reports that 50-70% of women experience back pain while pregnant. As your ligaments stretch and your pelvis widens, you will feel some discomfort in the first trimester. As your belly grows, the center of gravity shifts and this causes increased strain on your lower back. Anything more than just discomfort should be addressed right away. Sciatica is one of the more common diagnoses during pregnancy. A lot of times it could be pelvic girdle pain that is misinterpreted as sciatica. It would help to do some strengthening of your hip muscles to improve stabilization in your pelvis and reduce the pelvic girdle pain.
2) What exercises can be done during pregnancy to reduce low back pain? Do’s and Don’ts.
Exercises done during pregnancy should focus on hip strengthening, and gentle stretches for the lumbar spine, hamstrings, adductors, and glutes. Prenatal yoga is usually safe to perform.
Do not perform any abdominal exercises like crunches or sit-ups, as it might make your diastasis worse, and to be honest — there is a very little chance that you will get 6-pack abs while your belly is growing. If you have been a runner prior to pregnancy, you can continue running, but be careful in your 1st and 3rd trimester. A belly belt/support should be worn or Kinesio-taping should be done to prevent diastasis during your prenatal and postpartum journey.
Other good measures to take are strengthening your upper body during breastfeeding, as you most likely will have poor posture that might lead to upper back and shoulder pain. Maintaining good posture during pregnancy with postural awareness, strengthening, and stretching is a MUST. Though the Kegel is a good exercise to start during pregnancy, it is not always advisable for all pregnant patients. People suffering from vulvodynia, dyspareunia, or pelvic pain should focus on reverse Kegels and relaxation more than performing regular Kegel exercises.
3) Am I at risk for gestational diabetes?
Doing regular, gentle exercises, and walking can prevent gestational diabetes. So just remember to stay active during your pregnancy, and you should be good to go!
4) How do I stop urine from leaking when I don’t want it to. And when should I go to the doctor/physical therapist?
Performing pelvic floor strengthening is not just in the form of Kegels but other strengthening methods integrated with core strengthening can prevent leakage.
If you notice any pressure in your vagina, any bulging from your vagina while passing urine or otherwise, you will need to consult your physical therapist or OBGYN to rule out pelvic organ prolapse. If the leakage of urine has prolonged for more than 6 weeks postpartum and is getting worse, then you need to see your physical therapist.
5) You guys can improve scar tissue? What benefits does that have besides aesthetic reasons?
Physical therapy can help with scar tissue mobility for C-section scar, episiotomy scar, or scarring from a 1st-3rd degree tear. Scar tissue causes fascial restriction, which means it can adhere to the surrounding soft tissue and organs. This will often cause pain, poor extensibility, and decreased strength in the area.
You should wait until 6 weeks postpartum to start massaging or mobilizing your scar tissue.
6) How can I get rid of this split down my ab muscles?
That split or gap is known as Diastasis Recti, which is the separation of the abdominal muscle. During pregnancy, the uterus moves up into the abdomen and stretches between the rectus abdominis muscles to make room for the growing baby. Diastasis Recti can cause low back or pelvic pain but don’t worry, a physical therapist can help in reducing this separation through soft tissue mobilization in the abdomen, strengthening techniques, and even breathing techniques!
Some things to remember during pregnancy to avoid diastasis are: do not perform abdominal crunches and use Kinesio tape or a belly support belt during your 2nd and 3rd trimesters.
Here’s how to perform a self-test at home to see if you have Diastasis: Lay on your back, lift head off the ground, leaving your shoulders resting. Take your fingers and feel down the central abdomen, beginning at the sternum and travel all the way down while assessing that central line until you hit your pubic bone. While feeling down the midline, here’s what to look for:
- How wide is your separation?
- How deep is it?
- Can you feel the walls on either side of the separation?
- Is there any bulging in your central abdomen as you lift your head? (if you do see bulging, it is a sign that there is significant weakness in the deep layers of the abdomen)
7) Sex hurts. Will it always be like this? When does the pain go away?
This is known as Dyspareunia, which is a recurrent pain that is often located in the genital area and may occur before, during, or after sexual activity. This pain might come on as a result of the way your body changes during pregnancy, infections/STIs, vaginal dryness, or just stress. But luckily there are things you can do at home, or we can do to help Dyspareunia. Simple stretches like child’s pose, happy baby, along with diaphragmatic breathing and pelvic floor relaxation can go a long way. Pelvic floor massages and the trigger point release method using your finger, pelvic wand, or a miracle ball can help your symptoms as well. Pelvic wands and miracle balls are available online for purchase, however, we would not advise using these during pregnancy.
8) What is Pubic Symphysis Dysfunction and how do I know if I have it or am at risk for it? What can help these symptoms?
Pubic Symphysis Dysfunction is when your ligaments that normally keep your pelvic bone aligned during one’s pregnancy become too relaxed and stretchy after childbirth. This causes the pelvic joint – or symphysis pubis – to be unstable and which in turn, causes pelvic pain. Some symptoms include difficulty while walking and pain in your pelvis, typically focused in the pubic area but can also radiate towards the upper thighs and perineum. This doesn’t only happen while walking, but can happen while one is lifting heavy items, climbing stairs, getting dressed, getting into your car, or even while in bed.
You can do many things to ease your discomfort. We would recommend Hip stabilization exercises during pregnancy and also using an SI loc belt. Avoiding triggers is also important, this includes keeping your knees together during transfers like getting out of a car or getting out of bed, sitting down while getting dressed, and avoiding heavy lifting.
9) Why do I need a Pelvic PT for my pre-natal/post-natal care when I already have an OB/GYN that I go to?
An OBGYN is usually the first doctor people think of when it comes to prenatal care, delivery, and the postpartum journey. However, they usually aren’t trained to address the musculoskeletal implications like a Physical Therapist is. A Pelvic Floor Physical Therapist is even more apt to treat your pains and discomforts if you are pregnant, just gave birth, or just have any pelvic pains that might be also causing your abdomen, back or hip pain. However, not all OBGYNs will know when to refer their patient to a Pelvic Floor Physical Therapist, which is why often we encourage people to ask for a referral from their physician themselves. Some OBGYNs still may not give a referral, but you can always come straight to us and we can give you a free consultation!
No one deserves to live in pain, and the best way to help it is to prevent any further complications from happening. We believe in Preventative health as much as Reactive health, which is why seeing a Pelvic Floor Physical Therapist is important, especially while pregnant, to prevent any pain or conditions from happening in the first place. Here’s to healthy pelvic floors, and tearing down the stigmas that often surround Women’s Health issues!
Do you pee when you laugh? Or often feel like you won’t make it to the toilet on time?
That might be Urinary Incontinence. Urinary Incontinence is any undesired leakage of urine and the loss of bladder control, which is a common problem that affects both men and women. According to the American Urological Association, one-quarter to one-third of men and women in the United States experience Urinary Incontinence.
There are different types of Urinary Incontinence which includes:
- Stress Incontinence – urinating when putting pressure on bladder by coughing, sneezing, exercising, laughing, or lifting heavy.
- Urge Incontinence – having an intense urge to urinate, followed by involuntary loss of urine. Includes urinating throughout the night.
- Overflow Incontinence – having frequent dribbling of urine because of a bladder that doesn’t empty completely.
- Functional Incontinence – physical or mental impairment that prevents you to be able to get to the toilet on time. An example is arthritis that gets in the way of
- Mixed Incontinence – experiencing more than one type of incontinence, as listed above.
There is a long list of factors that can cause it, which includes childbirth, abdominal weakness, diabetes, pregnancy, menopause, and more. It can also be an uncomfortable topic for some, despite it being a widespread condition! Those who are pregnant may also experience persistent Urinary Incontinence due to hormonal changes, and the growing weight of the fetus which can lead to stress incontinence.
But you don’t have to live in pain. Did you know physical therapy can actually help? Specifically, seeing a Pelvic Floor Physical Therapist. A Pelvic Floor PT can help you create an individualized treatment program to help you improve your pelvic-floor muscle function. One can also help you improve control over your symptoms, as well as reduce the need for pads or incontinence medications, or even surgery! It’s much more than muscle strengthening when it comes to overcoming your Urinary Incontinence, it could also be about coordination, muscle imbalances, incorrect posture, core weakness, or even tight, overly active muscles.
Give us a call today if you or someone you know is experiencing or has been diagnosed with Urinary Incontinence and let’s figure it out together.
And how can it help you?
An Orthopedic Physical Therapist specializes in treating conditions that affect your musculoskeletal system. It involves many hands-on techniques, manual therapy, and exercises to improve many things – such as flexibility and strength of muscles, increasing range of motion of joins, reducing inflammation in joints and tendons, as well as reducing scar tissue post-surgery. This means that Orthopedic PTs can treat almost any condition that affects your ability to move or physically function in your everyday life.
What does your musculoskeletal system include? It includes your ligaments, tendons, joints, muscles, bones, and all connective tissue.
So what are some conditions that affect the musculoskeletal system?
- Arthritis
- joint pain
- knee instability
- limited range of motion
- lower back pain
- frozen shoulder
- scoliosis
- stroke
- plantar fasciitis
- muscular dystrophy
Orthopedic Physical Therapists also help a lot of patients who are recovering after surgeries. This is to help reduce pain, improve walking or a limited range of motion, and scar tissue.
Patients often need an Orthopedic PT after surgeries/injuries like:
- rotator cuff repair
- knee replacement
- hip replacement
- herniated disk
- sprained ankle
- torn meniscus
- shin splints
- tennis elbow
- carpal tunnel
So don’t wait to get checked up by an Orthopedic certified Physical Therapist. One can analyze your movement to find the source of injury or problem. They can improve pain, swelling, stiffness, immobility, as well as give you advice on preventing injuries in the future.
If you suffer from any of the aforementioned problems, give us a call today to get treated by Dr. Mathew.
Fun Fact: Did you know she has been awarded the Orthopedic Clinical Specialist (OCS) certification by the American Board of Physical Therapy Specialists? A specialization that requires thousands of hours of training and is earned by only 5% of Physical Therapists across the country.
If you or someone you know has ever suffered from pain during sex, sitting for a long amount of time, or wearing tight pants, you might be scratching your head as to the root of your pain. You may think it’s a urinary tract infection, or maybe even an STD. But when the tests are negative, you and your healthcare provider may not be aware that this pain could be thanks to musculoskeletal dysfunction, which can be treated by a pelvic physical therapist.
Your pelvic floor is a set of muscles that support the bladder, bowel, rectum, and uterus. Pelvic floor pain is something that is not talked about enough in our everyday lives and on social media. Women can suffer from pelvic floor pain, and not even know it! In many cases, bladder, bowel, or pelvis symptoms may be occurring due to problems with the muscles, joints, nerves, or connective tissues in that area.
Pelvic floor physical therapy can help with many different kinds of problems including:
- Frequent urination
- Urgency: Strong urge to urinate
- Incontinence: Unwanted leaking of urine or stool
- Constipation
- Overactive or weak pelvic floor muscles
- Endometriosis
- Menopause
- Pain in the pelvis, hip, abdomen, low back
- Painful intercourse
- Sexual dysfunction
- Pregnancy/post-pregnancy pain or intercourse
- C-section recovery
- Pelvic Organ Prolapse
- Vulvodynia
- Bladder pain syndrome
- Tailbone Pain
- Postsurgical rehabilitation
These symptoms may be caused by the strength of the pelvic floor and associated muscles and structures. Thus, the movement, muscle tone, and strength of your low back, hips, abdomen will be assessed, together with your posture and alignment. Pelvic floor physical therapists can treat many different conditions and can help you keep your pain in check. Women need to know that pelvic pain isn’t normal during menopause or any other time. Also, the longer one experiences chronic pain, the more likely nerve receptors will become sensitized to it.
Here at New York Plaza Physical Therapy, we wish to open that dialogue about the countless people, especially women, who suffer from pelvic pain and provide some treatment options to assist them in living a pain-free life. We understand that the implications of pelvic pain going unnoticed or unchecked can deeply affect one’s quality of life. So if you’re stricken by unexplained chronic pelvic pain or any of the above symptoms, it may be wise to give us a call today.
References:
Harvard Health Publishing. (2020, October 13). Pelvic physical therapy: Another potential treatment option. Retrieved from https://www.health.harvard.edu/womens-health/pelvic-physical-therapy-another-potential-treatment-option
Tate, L. (n.d.). What in the World is Pelvic Floor Physical Therapy? Retrieved December 18, 2020, from https://www.pennpartners.org/blog/expertise-general-outpatient-therapy-pelvic-floor-physical-therapy-specialty/what-world-pelvic
WHETHER YOU’RE BACK IN THE OFFICE OR WFH, THESE CAN EASILY BE DONE FROM ANYWHERE 👩💻
Work-related injuries aren’t limited to people who work with heavy manufacturing or construction. They can occur in every industry and work environments, including office spaces. Studies have proven that repetitive motion, poor posture, and staying in the same position for long periods of time can cause or worsen musculoskeletal disorders. Make sure to take a break every hour or so to stretch out and move your body.
Below are some easy exercises anyone can do at the workplace!
Cervical Retraction
These movements are meant to correct forward head posture. You are retraining deep cervical flexors while maintaining mobility in the cervical spine. This will prevent disc herniation and degeneration.
Lumbar Extension
This exercise prevents lower back pain. Sitting causes increased rounding of the lumbar spine and increased risk of disc herniations. The extension helps maintain mobility in the spine.
Scapular Retraction
Here we use shoulder blade pinching to correct slouching posture. Bring your shoulder blades together, hold for 5 seconds, and relax.
Wrist Flexors
Do you want to prevent Carpal Tunnel Syndrome and Tendinosis of the wrist? All you need to do is hold each stretch for 20 seconds.
5 Simple Ways To Prevent Back Pain
A study shows that 3/5people suffer from either neck pain or back pain or both.
A recent study from American Journal of Public Health, reveals that 1 hour of siting = 1 cigarette..
Here is a chart that will give you an insight on how much pressure falls on the disc during various activities that we carry on during the day. Unsupported sitting put maximum pressure on the spine which results in pain.
Symptoms of back pain depending on the severity of your condition:
- Centre back pain
- Pain radiating to either or both legs
- Tingling or numbness in either or both legs
- Weakness of leg muscles
How can you prevent pain & treat yourself:
- Maintaining a correct posture
- Using a Lumbar roll while sitting
- Taking adequate breaks – every 30mins for 30seconds
- Bend from the knees not back
- Strengthening your spinal muscles
We bend about 7000+ times a day which loads the spine more leading to back pain.
This simple exercise can help you alleviate the pain and relieve the extra stresses that fall on the spine.